Water and Sanitation
A little more than a hundred years ago, diseases such as typhoid and diarrhea were the third major cause of death accounting for 10% of all deaths. Outbreaks were often attributed to water supplies contaminated by human waste. Few piped water systems had any treatment, and disinfection with chlorine was yet to be discovered. Similarly examining the water for bacterial indicators of contamination was not common until the late 19th century.
Access the MCN - Farmworker Justice Guide to OSHA's Field Sanitation Standard for Clinicians
Despite advances in water supply and treatment, many farmworkers remain vulnerable to contaminated water supplies. Most of the water sources used to provide water to farmworkers in the fields or in the camps are private wells. These supplies are not regulated under the federal Safe Drinking Water Act of 1974 as this law applies only to systems serving 25 or more people for at least 60 days per year. Further, only a handful of states have regulations in place, which cover these smaller systems or systems specifically serving farmworkers. As a result a very small proportion of these wells are tested for microbiological or chemical contamination, and few are inspected to assure that the source waters are protected from contamination.
This is of particular concern in agricultural areas where rain and irrigation water can carry pesticides, fertilizers and human and animals wastes through the soil and into the underlying aquifer. It is these aquifers that are tapped by the shallow domestic wells typically used to provide drinking water to farmworkers in the fields and at labor camps. A recent study by the US Geological Survey showed that nitrate, found in fertilizers and animals wastes, was the most commonly found contaminant of wells.
Historically, water and sanitation problems have had a significant impact on farmworker health. Studies dating back to the early 1980s have documented high levels of enteric disease and poor sanitary conditions (Ortiz, 1980). Arbab and colleagues (1986) found that migrants displayed a clinic utilization rate for diarrhea 20 times higher than that of urban poor. In a North Carolina study Ciesielski et. al. (1992) found a high prevalence of intestinal parasites, and an association between having parasites and poor sanitary conditions. Moreover, a 1988 EPA study conducted in Wisconsin found that sanitation problems increased during the summer months when more workers are in the region. Wells tested in May showed no signs of microbiological contamination, where as nearly 50% of the wells tested in July tested positive for microbiological contamination.
While more recent information from National Agricultural Worker's Survey and the California Worker Health Survey in 1999 indicates that there have been significant improvements in field sanitation, there are still troubling reports that water and sanitation problems remain a concern. In a 1999 sanitary survey of wells serving temporary farmworkers and their families in the Washington State, 101 out 179 wells showed problems and 23 of the wells obtained water from unacceptable sources. A recent series of focus groups conducted with farmworkers in Washington State found that water and sanitation continues to be problematic both in the field and at housing sites (Washington State Department of Health, 2002).
There are two important aspects for clinicians to understand regarding water and sanitation. 1) While pesticide and nitrate contamination of water is a problem, fecal contamination is a primary source of enteric disease. 2) Enteric disease is not only water-borne, but transmitted through fecal-oral routes of transmission.
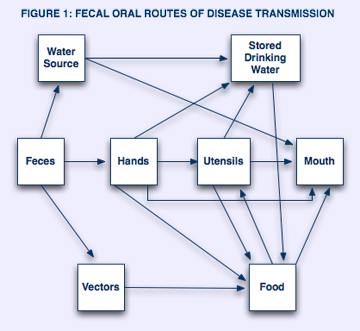
Figure 1 provides a simplified illustration of the various routes of fecal-oral transmission. This diagram shows that fecal contamination of water, hands, and the environment sets the stage for transmission of disease. The following are all methods for disease transmission:
- Water sources may be directly contaminated (i.e. a poorly maintained latrine or septic system can contaminate water wells).
- Stored water can be contaminated through contact with contaminated hands or utensils.
- Contaminated water may be ingested directly or used to wash dishes andutensils or to prepare food.
- Contaminated hands may directly contact the mouth, drinking or cooking water, utensils, food etc.
- Vectors such as flies may also contribute to the transmission of disease as contact both feces and food. (Actions Speak, 1993).
Farmworkers and their families often live and work in settings where there are multiple routes of transmission as described above. Farmworkers may or may not be exposed to contaminated water via poorly maintained wells. Facilities for hand washing and properly maintained excreta disposal systems may or may be available to farmworkers. Knowing that enteric infection may be an issue for farmworkers has several implications for clinicians, outreach workers, and health educators.