The Risk... Talking to Patients about Pesticides

During a prenatal check-up, an agricultural worker patient asks a question about the mosquito control in her neighborhood: “They are fogging by airplane in our community occasionally at night. I close the windows, but is it safe the next morning for my young children, and for me? Should we stay at my sister’s house when they spray?” Clinicians are often taxed with answering pesticide safety questions with limited information and training — but a careful and clear informational approach, supplemented with reliable resources the patient can access, can help patients understand their pesticide exposure risk and make informed behavior changes if they determine their risk is high.
Approaching the Conversation with Risk in Mind: A Checklist
For a comprehensive approach in the exam room, we turn to the National Pesticide Information (NPIC). A cooperative agreement between the Environmental Protection Agency and Oregon State University, NPIC answers over 11,000 calls and emails from the general public each year about pesticides. Their goal is to help people understand their risk through objective, science based information about pesticides and related topics. Their conversations usually contain the following elements, all of which are applicable for patient-provider conversations as well.
1. Risk — not Safety
It’s critical to frame the conversation in terms of a patient’s risk, not their safety, says Amy Hallman, MS, Project Coordinator of NPIC. “The safety question is the same for every person,” Hallman explained during a recent NPIC webinar. “Is it safe?” can end up being a yes or no answer. “Risk, however, has lots of factors that may make something more or less risky,” Hallman said, depending on their personal circumstances, so a focus on risk can lead to a well-rounded discussion that is tailored specifically to the circumstances of the questioner. If a clinician gives the patient the impression that a given pesticide is safe, however, “it can lead to careless behaviors, or lack of vigilance, which can increase their risk,” Hallman noted, and the “safe” pesticide may no longer be safe.
Risk is a combination of the toxicity of a product and the amount of exposure. Exposure can vary greatly. When mosquito fogging occurs, the toxicity of the pesticide remains constant, but the exposure is different. A pregnant woman with a young toddler whose toys are outside will have a different risk than a single male living in an apartment in the same area, because her potential for exposure is greater. Patients may not be able to control the toxicity of a product — especially agricultural workers, who may be exposed to numerous products at their workplace — but they may have greater control over their exposure.
2. Listen, ask questions, and paraphrase
Just as in all of our conversations with patients, a complete and detailed conversation about their physical situation and their past experiences can help us better understand their needs and exposures. What type of features in their environment may increase their risk — is there a barrier between the yard and the field next door? Is there a windbreak that reduces drift? Habits of the individual and family may also affect their risk. Does the patient utilize personal protective equipment (PPE) every time, or does the patient skip it if it’s too hot outside? Does the patient wash hands and change his clothes after returning home and before hugging his children? Are shoes allowed in the house?
Hallman notes that perceived risk may not match actual risk. Clinicians may need to delve deeper into a patient’s experiences and values to unearth how patients perceive their risk of exposure. Hallman outlines factors that influence a person’s risk perception. The chemical may be viewed as:
- Out of a person’s control or imposed versus in a person’s control or voluntary;
- Beneficial versus damaging;
- Natural versus manmade;
- Only affects adults/has no effect versus affects children;
- Unfamiliar and untrusted versus familiar and trusted.
Many clinicians have seen this with agricultural worker patients. If an agricultural worker has applied chemicals many times before, he may not perceive his risk as high because the application is routine and familiar, and he has not experienced any acute reactions. Alternatively, a worker who is new to agricultural work may find chemical application concerning, when the routine and the product are untrusted and unfamiliar.
To assure that the patient feels their concerns and needs are heard, clinicians can reiterate the patient’s concerns back to the patient.
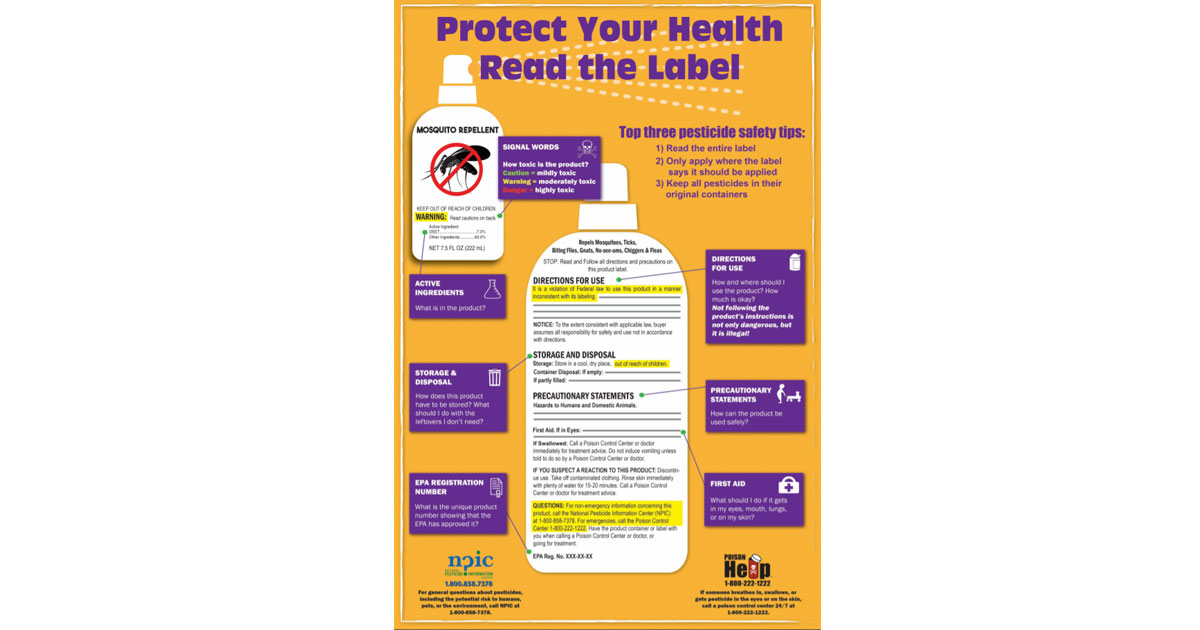
3. Toxicity Information: Understanding Signal Words
Another key aspect of the conversation can be around the product itself. Helping a patient understand a product’s label can help them understand the risk. Critically, product formulation varies from product to product and requires the user to pay close attention to precautionary statements and instructions for use. The active ingredient by itself may be highly toxic; the formulation of the product with the active ingredient may or may not be.
Hallman places emphasis on the signal word. The product will be labeled with a signal word designated by the Environmental Protection Agency that is specific to the formula: CAUTION, which indicates mild toxicity; WARNING, moderate toxicity; and DANGER, for high toxicity. A signal word is determined by evaluating all active ingredients for toxicity through each route of exposure — acute oral or dermal lethal dose, inhalation lethal concentration, primary eye irritation, and primary skin irritation. The product will carry the signal word of the highest category of concern, regardless of route of exposure. For example, if a product is corrosive to the eyes indicating high toxicity for eye exposure, but the product is low in toxicity for all other routes of exposure, it will still carry the DANGER label to indicate that at least one route of exposure can result in serious injury. If a product is considered low in toxicity for all routes of exposure, then the product will carry the CAUTION signal word.
In many cases, however, a patient may not have the product with them or have access to the product. In this case, a clinician can still have a valuable conversation about how to reduce risk, even when the product toxicity is unknown.
4. Exposure Information: Action Items
After the clinician has a greater understanding of the patient’s perceived risk, his or her environment, the toxicity of the product, and how it will be applied, the clinician can now recommend action items in the patient’s control that will limit the patient’s risk of exposure. For our pregnant agricultural worker and her children, this may include bringing in toys and removing hanging laundry for the night, closing windows, covering the vegetable garden for the night, and more vigilance around shoe wearing in the house. It may be a good time to check in on other possible exposures at work that the patient may have not been concerned about because of a perceived low risk.
Clinicians may refer the patient to trusted, science-based information sources outside of the exam room. NPIC’s website features fact sheets, FAQs, podcasts, and videos that are developed based on emerging concerns and on the frequently asked inquiries they receive via phone and email. Access NPIC’s resources at: http://www.npic.orst.edu/. NPIC’s “Is It Safe?” Fact Sheet is at: http://npic.orst.edu/factsheets/isitsafe.html. Their Reading Pesticide Labels Infographic is at: http://npic.orst.edu/outreach/labelinfographic.pdf. Watch the webinar for more information on communicating with the public about pesticides: https://youtu.be/RRinp6IMH8g.
Should the patient’s concern about an exposure be workplace-related, clinicians must report the incident in most states. Please refer to MCN’s Pesticide Reporting Map to see reporting requirements and recommendations for your state: https://goo.gl/ttknSD.
Read this article in the Fall 2017 issue of Streamline here!
Sign up for our eNewsletter to receive bimonthly news from MCN, including announcements of the next Streamline.