
Health inequities are rampant in the United States. Black women are more likely to die from giving birth than other women, even when other factors like income and education are accounted for.9 Migrant agricultural workers move every few weeks for the harvest, often crossing state lines; if eligible for health care, they must reapply in every new state, an almost impossible bureaucratic burden. A person diagnosed with diabetes who is told to eat fresh vegetables and get more exercise, may live in a community unsafe for exercising outside, and only have a convenience store for food. From rates of morbidity and mortality, to access to quality health care, to services in one’s preferred language, to the social determinants that remain unaddressed, most health systems generate or perpetuate racial, social, economic, and/or health inequities that negatively impact the health and well-being of underserved and historically marginalized people, including agricultural workers. The efforts to shift health systems to be more equitable, however, often fail to include the communities that those systems serve. Community participation, posit the authors of a new conceptual model, is key to such efforts. To meaningfully build health equity, systems of health must be transformed through efforts that center firmly around community, and community engagement.
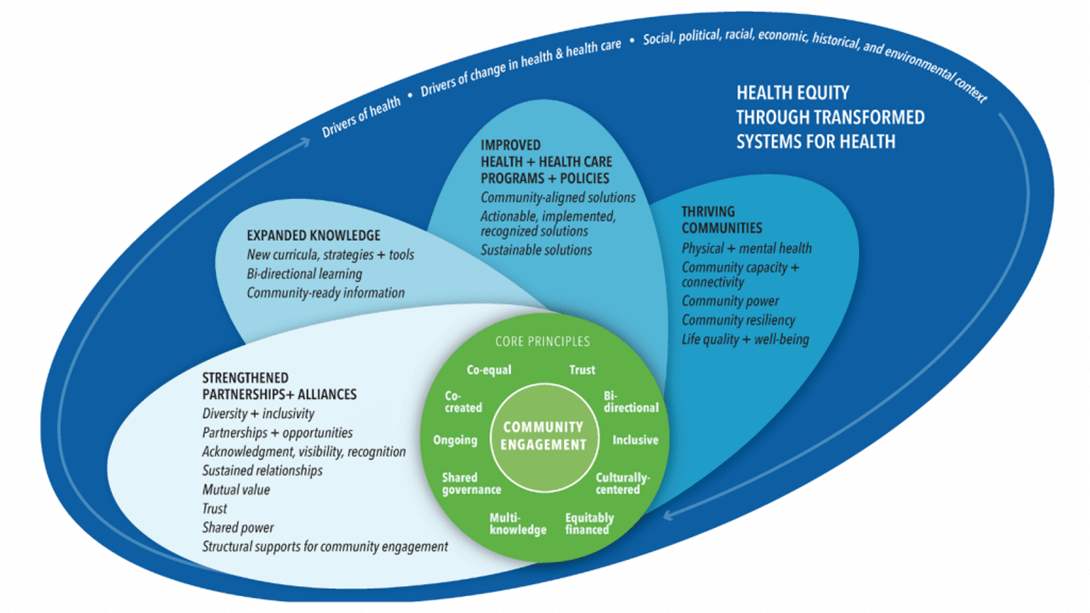
Achieving Health Equity and Systems Transformation through Meaningful Community Engagement, also known as the Assessing Community Engagement (ACE) Conceptual Model, encourages community efforts to focus on four “petals” or “propellers” of measurable outcomes that grow out of community engagement: strengthened partnerships and alliances, expanded knowledge, improved health and health care programs and policies, and thriving communities.10 A community can utilize the outlined domains and indicators related to each petal to encourage meaningful engagement on their health equity goal, say the authors. A commentary introducing the model was published in February 2022 in NAM Perspectives, from the National Academy of Medicine.
The authors sought to build an efficient and useful model that would:
- Define what should be measured in meaningful community engagement, not what is currently measured;
- Be sufficiently flexible to measure engagement in any community;
- Define health holistically;
- Allow the community to see itself in or identify with the language, definitions, and context.
- Embed equity throughout the model;
- Emphasize outcomes of meaningful community engagement;
- Present a range of outcome options for various stakeholders; and
- Communicate the dynamic and transformative nature of engagement.
The authors found that existing conceptual models lacked flexibility for various community partners and sectors, and the norms, needs, and processes that those partners bring. Few made the connection between community engagement and outcomes or metrics, and none examined how community engagement could impact health care policies, particularly with the incorporation of diversity, inclusion, and health equity, the authors concluded. This model, with community engagement at the center, allows for meaningful, lasting, and connected community health interventions and policies.
The model reflects the community-centered ethos that many health equity-focused groups like Migrant Clinicians Network have relied on and advocated for, for decades.
“The community mobilization model, the participatory research and evaluation approach that MCN utilizes – it is all encompassed in this conceptual model,” noted Alma Galván, MHC, Senior Program Manager with MCN, who celebrated the model, and noted it was developed by well-respected leaders in the field.
The model validates and elevates the approach that MCN has relied on, and emphasizes to funders the need for long-term support of the infrastructure and relationship-building that such a model relies on. When COVID hit, Galván noted, many community-based organizations were eligible for significant new avenues of funding around COVID – but as the pandemic wears on, funding has evaporated. Yet, relationships forged in this emergency should be maintained. Healthy mutual relationships between organizations and their communities can support the health of the most marginalized, either during the next infectious disease emergency, or to address chronic ongoing health concerns like diabetes. For overlooked communities like migrant agricultural worker communities, such relationships are essential.
“To build health equity, it’s not just about the health challenges agricultural workers have as individuals, but about the structural challenges in this country, the laws that do not help them, that keep them from having access to services, and to health information,” Galván said. “It is not an easy solution – and it takes time. But to move the needle on the structural challenges that they have – like immigration status, health system access – you need to go through the process to build the trust.”
Read the journal article on the conceptual model: https://bit.ly/3ms84uf.
9 What Are Maternal Morbidity and Mortality? Maternal Morbidity & Mortality Web Portal. National Institutes of Health. https://orwh.od.nih.gov/mmm-portal/what-mmm
10 Organizing Committee for Assessing Meaningful Community Engagement in Health & Health Care Programs & Policies. 2022. Assessing Meaningful Community Engagement: A Conceptual Model to Advance Health Equity through Transformed Systems for Health. NAM Perspectives. Commentary, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/202202c.
Read this article in the Summer 2022 issue of Streamline here!Sign up for our eNewsletter to receive bimonthly news from MCN, including announcements of the next Streamline. |