
In California’s San Joaquin Valley, dangers lurk in the air. The valley, the southern half of California’s Central Valley, and an important agricultural region with billions of dollars of annual agricultural output, struggles to meet federal air quality standards, with topography, agriculture, industry, and heat each contributing to the Valley’s poor air quality. During the summers, agricultural workers may toil in the fields or orchards in extreme heat, breathing in very high ozone concentrations, wildfire smoke, and dust and other particulate matter. But San Joaquin Valley is not an anomaly – it is an agricultural harbinger. As climate change, environmental degradation, and industrial agricultural practices continue, the air quality of agricultural basins across the United States may see more extreme heat, coupled with the poor air quality days that San Joaquin already experiences frequently. And the health consequences for low-income migrant and immigrant agricultural workers – who experience additional factors that increase the health risks of these exposures – are worse than for the general population. Here, the primary environmental factors that contribute to poor air quality are outlined, followed by two critical health factors – diet and stress – that agricultural workers typically face, that further impact their respiratory health and ability to recover when exposed to a respiratory stressor like COVID.
Ozone and Particulate Matter
Ozone is created when ozone precursors like carbon monoxide, methane, and nitrogen oxide are released into the atmosphere by motor vehicles, power plants, and industrial processes. These chemicals react with solar radiation to form ozone. San Joaquin Valley has exceptionally high ozone levels.
“Ozone is one of the primary pollutants in smog in California,” explained John Balmes, MD, a physician member of the California Air Resources Board. Because of its topography, the San Joaquin Valley is particularly susceptible to air pollutants like ozone; pollutants are blown down the Central Valley and get trapped under the San Joaquin’s sunny skies. Climate change is slated to worsen ozone in the region, despite efforts in recent years to reduce it.
“Between cleaning up motor vehicles and [increasing the use of] renewable energy, there are fewer precursors for ozone,” noted Dr. Balmes. “But it’s still a problem. There’s a direct relationship between how hot it is, and how much ozone there is.” As the San Joaquin Valley gets hotter, ozone’s threat on agricultural work increases.
“It’s pretty toxic to the airways,” Dr. Balmes explained. “It chemically burns the lungs, and that can cause even healthy people to have some respiratory symptoms, especially if they’re exercising – breathing through their mouth, breathing harder, and more per minute. Construction and farm workers have the highest exposure. Even if they’re healthy, with no health conditions, they can get symptoms.” Short-term exposure to ozone can reduce lung function and cause an inflammatory response in the airway.1 Patients may experience reduction in forced expiratory volume, shortness of breath; throat irritation; coughing or wheezing; or pain, tightness, and/or burning in the chest. Reaction to exposure varies greatly; one patient may experience no symptoms or lung function changes, while another person exposed to ozone in the same concentration and time duration will experience a 50% decrement in forced expiratory volume in one second (FEV1) and significant and disruptive symptoms.2
Chronic exposure to ozone results in impaired development of lung function in children. “We worry that kids that grow up in polluted areas and have lower lung function in early adulthood are at greater risk for respiratory problems later in life,” Dr. Balmes explained. Chronic exposure to ozone, regardless of age, is linked with asthma. Those already diagnosed with asthma or other pulmonary disorders like bronchitis or emphysema are more likely to experience health effects from pollution exposure.
Air pollution in the San Joaquin Valley is not limited to ozone, however. Fine particulate matter (PM2.5), airborne particles that are 2.5 micrometers or smaller, is released into the San Joaquin air from sources like agricultural equipment, residential wood burning, and commercial charbroiling.3 The Fresno region – the Valley’s largest city -- is ranked as having the worst PM2.5 rates among metropolitan areas in the country.4 The impact of PM2.5 exposure is similar to that of ozone, and the two have often been studied simultaneously. In 1992, the Children’s Health Study from the University of Southern California began to track the respiratory health of children from fourth to twelfth grade, charting their health against the ozone, nitrogen dioxide, and PM2.5 levels in their neighborhood. By age 18, those children growing up in more polluted areas had underdeveloped lungs.5
Since then, the study, along with many others, has connected air pollution exposure to health consequences beyond the lungs. Contaminants, researchers found, enter the circulatory system from the lungs and have effects on the heart, brain, and metabolic system.6 For example, when air quality is poor, cardiovascular events increase, and adults are more at risk of type 1 diabetes.7 Air pollution impairs white blood cells in the lungs, which reduces the body’s ability to mount an effective immune response or induces a shift in white blood cell immune responses toward allergy. 8,9
Pollution in the Age of Climate Change
Yet, these significant health risks from PM2.5 and ozone are now being accompanied by new factors: wildfire smoke and excessive heat. California is rapidly changing, as climate change drives drier conditions, prolonged droughts, and unprecedented heat, with both higher temperatures and longer duration of heat waves.
The pollutants in wildfire smoke are dangerous, but the specific long-term consequences of repeated exposure that agricultural worker families are now experiencing every year in San Joaquin Valley have yet to be quantified. “Young children who experience, every year, a fire season – there’s a concern, but no evidence at this point, that they are at greater risk for respiratory problems later. We just don’t know yet, for wildfire smoke,” Dr. Balmes said. But the data are accumulating. A 2021 study determined that wildfire smoke increased the risk of preterm birth in California.10 Other studies point to increased risk of respiratory, mental, and perinatal health concerns, and possible cardiovascular consequences as well.11-14 Premature mortality resulting from wildfires is only expected to grow as the climate crisis progresses.15 The climate crisis is expected to increase the number of wildfire-related smoke days in the US, particularly in the West and Great Plains.16 When a new respiratory disease arrived – COVID-19 – those exposed to wildfire smoke were predisposed to poorer outcomes. A 2021 study found that there were an estimated 20,000 additional COVID-19 infections and 750 COVID-19 deaths associated with exposure to wildfire smoke in the West in 2020.17
Heat is also on the rise due to the climate crisis, which in turn exacerbates the pollution crisis. Extreme heat days are associated with high ozone. Ozone production accelerates at high temperatures, and in the Valley, extreme temperature days are frequently associated with high air pressure and no wind, which prevents air pollution from being swept out of the Valley. Already, the San Joaquin Valley experiences more heat than in the past. In 2021, Fresno experienced 69 summer days above 100 degrees – a stark difference than the average of 10.3 days above 100 for the Valley, between 1961 and 1990.18,19 And its heat is projected to significantly worsen. Its four to five average extreme-heat days – those over 104 degrees – will increase to 18 to 28 days by mid-century.20 (See sidebar on heat-related illness.)
Agricultural Workers Struggle to Avoid Exposure
The impact of pollution and heat combined are not evenly felt across the San Joaquin Valley. Farmworkers are particularly at risk for adverse effects of these exposures due to their workplace and lifestyle. Most farmworkers in San Joaquin Valley are routinely exposed to ozone, extreme heat, and PM2.5 while working outdoors, often completing high-exertion tasks while growing, harvesting, and packing fruits, vegetables, and nuts, which increases their susceptibility to the adverse effects of heat, ozone, and PM2.5 exposure.
Regulations to limit these exposures in California have had mixed results. California law requires employers to provide water, rest, and shade for agricultural workers in high-heat environments, but workers who are paid piece rate may find these breaks hard to take as they result in lost income (although, in California, mandated rest breaks must be compensated21). Some have complained that water and shade are provided too far from the area in which they are working to be effective. Additionally, agricultural workers often come to work already dehydrated, compounding the stress on their bodies.22 (See sidebar on an analysis of California’s heat regulation.) California’s 2019 emergency regulation to protect agricultural workers from wildfire smoke requires employers to provide N95 masks on poor air quality days. This regulation may be at odds with the realities of farm work; many agricultural workers may decide to forgo respiratory protection even in heavy smoke. Many workers find high-exertion work difficult while wearing a fitted respirator properly for hours at a time.23 Under the regulation, outdoor work must be suspended entirely when air quality dips into “hazardous” conditions, in which PM2.5 registers between 301 and 500 parts per million, but such a loss of income, even for one day, may cause severe financial strain. Agricultural workers often struggle to afford basic needs like housing and food, as most live in poverty and from paycheck to paycheck. What’s more, agricultural workers, due to poverty, immigration status, and language differences, may not want to voice concern over hazardous conditions that are regulated in California. Others wish to continue working, despite the health risks.
Exposures to heat and pollution do not end when workers leave the fields. Agricultural workers frequently live in substandard, poorly insulated housing without air conditioning or air filtration. This results in ongoing exposure to heat and pollution, even when sleeping at night. Ozone levels drop and wildfire smoke plumes sometimes shift when the sun sets, but pollution often continues at unhealthy levels at night, and temperatures in the San Joaquin Valley remain elevated even at night.
These social determinants place agricultural workers in positions that result in the inability to avoid exposure. Consequently, an agricultural worker’s body is constantly under stress from these physical exposures to PM2.5, ozone, and heat.
Exposomic Health: Taking All Exposures, Including Social Determinants of Diet and Stress, Together
The body’s stress from these external factors is enhanced by yet more damaging exposures including psychosocial stress, says Dr. Balmes. For example, experiencing racism raises baseline stress levels, which reduces the body’s ability to ward off the health consequences of physical stress-inducing exposures. “You can measure biomarkers of stress in people who experience racial discrimination, and you can see how air pollution affects those who experience it, versus those who don’t. Psychosocial and physical exposures – they’re synergistic,” Dr. Balmes noted. Baseline stress is also elevated by continuous concerns over finances. Consequently, low-income people of color like agricultural workers have increased susceptibility to respiratory distress because of the body’s persistent state of stress.24
Poor nutrition among agricultural workers further reduces the body’s ability to repair itself in the face of air pollutants. Agricultural workers suffer more than the general population from diet-related chronic health outcomes like obesity and elevated cholesterol. These health incidences point to diets low in antioxidant-rich fruits and vegetables. In addition to fending off these chronic health conditions, fruits and vegetables improve respiratory health. “Antioxidants actually protect the airways from being burned” by ozone and other pollutants, explained Dr. Balmes. Air pollution like ozone contains oxidants that create free radicals that injure respiratory tract cells, causing burns and inflammation. Inflamed and damaged lungs, in turn, are more susceptible to infection. “Antioxidants do exactly as they sound – they act against the oxidants.”
Scientists are just beginning to uncover the linkages between exposures and mechanisms like diet and stress that, over the course of a lifetime, lead to poor respiratory health. An “exposomic” approach takes into account all of these environmental, physical, social, nutritional, and psychosocial aspects of an agricultural worker’s life. As expected, it’s complicated. “Multiple pathways with complex interdependencies must be considered when examining the integrative influence of social, chemical, and physical environmental factors on respiratory disease,” notes a February 2023 journal article on advancing exposomic research in respiratory disease.25 Yet, these overlapping factors help clinicians tease out how agricultural workers are predisposed to poor health and premature death.
Solutions At Hand
Clinicians, including community health workers and outreach workers, have a significant role in pursuing and promoting solutions to the exposures that affect agricultural workers’ respiratory health.
Within the community, clinicians can design culturally contextual education to help agricultural worker communities understand the risks they take at work and the rights they have to protect their health. Training on practical approaches, from mask wearing, to nutrition, to home ventilation, is key to helping agricultural workers reduce their preexisting health risks before the next climate-induced heat wave, wildfire, and/or air pollution event. (See sidebar on Practical Approaches for some ideas.) As climate change progresses, ongoing relationships with agricultural worker communities are essential to ensure that trust and communication are high between the clinic and the agricultural worker community to build community mobilization and inclusion before a climate-fueled disaster strikes.26
At the clinic, a greater focus on reducing health disparities and addressing the social determinants of health may mean more emphasis on warm hand-offs to social workers, nutritionists, educators, and others who focus on reducing disparities.
At the state and federal level, clinicians can loudly voice the need for strong protections from heat and air pollutants, the need for improved management of forests to reduce the likelihood of megafires, and for bold and urgent action to reduce greenhouse gases. Migrant Clinicians Network regularly participates in these advocacy efforts and invites clinicians to join. Clinicians, as trusted members of the local medical community, can assist by providing context and understanding of the significant and worsening local health consequences of this global phenomenon.
Heat-Related Illness and Farmworkers
These excerpts are from the Heat-Related Illness Clinician’s Guide, developed jointly by Migrant Clinicians Network and Farmworker Justice. The Guide is available for download, in English and Spanish, on our website: https://www.migrantclinician.org/resource/heat-related-illness-clinicians-guide-june-2021.html
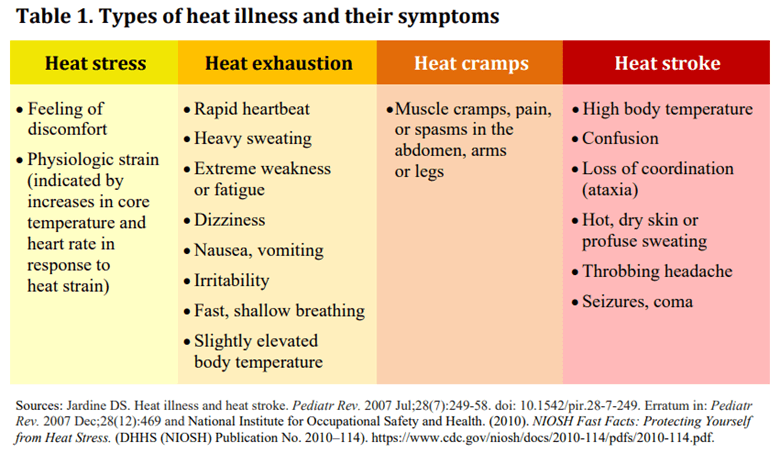
Agricultural workers are at significant risk for heat stress. Heat stress results when the body cannot get rid of excess heat and its core temperature rises. Heat stress may lead to more severe heat illness including heat exhaustion, heat cramps, heat stroke, and even death if left untreated. Agricultural work, which requires performing physically demanding work for long hours in hot and sometimes humid weather, places workers at high risk.
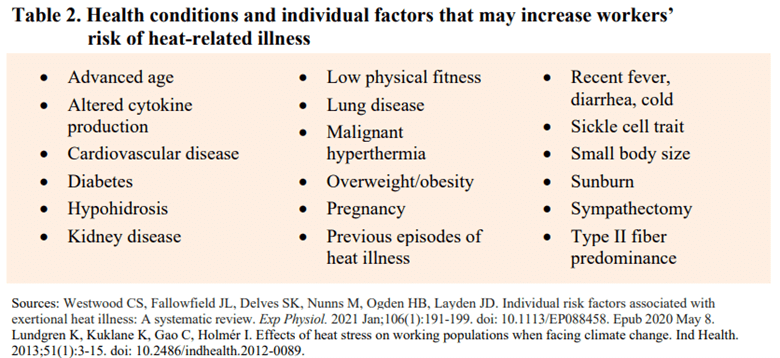
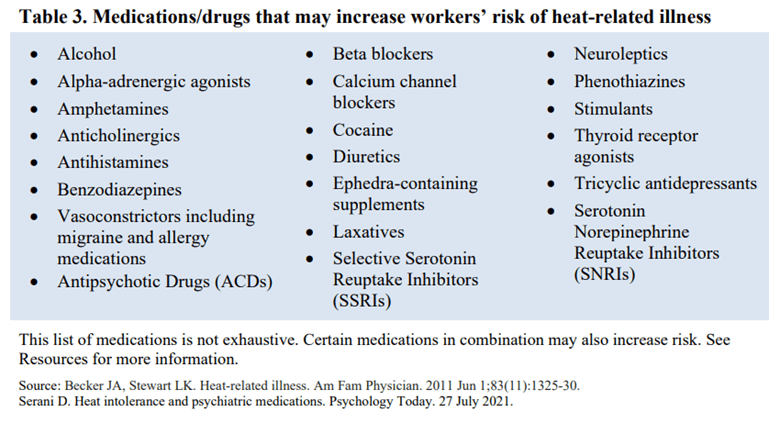
High environmental temperatures, humidity, low or no-wind conditions, sun exposure, dehydration and physical exertion are all risk factors for heat illness. Consuming alcohol or drinks high in caffeine—such as energy drinks—may increase the risk even further. Personal factors such as age, weight, pregnancy, physical condition and use of certain medications may also put workers at greater risk… Serious heat illness is also more common among workers who are not accustomed to working in the heat. Approximately 50 to 70 percent of deaths attributed to outdoor heat exposure happen within the first few days of working in a warm or hot environment, due to lack of acclimatization.
Risk factors such as past episodes of heat illness and medical conditions or medications that affect the body’s heat-regulation mechanism can make workers more susceptible to the effects of heat. Therefore, ascertaining a patient’s clinical history is a key step toward identifying those at higher risk… Physiological and pharmacological risk factors [additionally are] associated with a greater risk of heat illness.
The following three tables are taken from the Clinician’s Guide. The Guide includes additional sections on: chronic kidney disease of nontraditional origin; prevention, treatment, medical attention, and post-treatment follow-up; messaging and resources; social determinants of health; and heat-related illness and the law.
Practical Considerations on Farmworker Exposure to Respiratory Risks
N95 respirators during smoky days are difficult to tolerate when exerting one’s self. Encourage agricultural workers to use N95 respirators with an external valve, which may make heavy breathing more comfortable. The external valves are inappropriate for a clinical setting, or anywhere where COVID-19 spread is a concern, but work well in an outdoor setting when the goal is to reduce exposure to air pollution.
Air purifiers are expensive. Some air quality districts, including in San Joaquin Valley, offer programs to provide free or reduced cost air purifiers. Another option, says Dr. Balmes, is to secure a MERV-13 air filter over a box filter – likely less effective than an air purifier, but an inexpensive and effective alternative. One design, the Corsi-Rosenthal Box, utilizes 4 filters.27,28
California’s Heat Standard as a Model for the Nation
Only five states have regulations to protect workers from heat stress: California, Washington, Colorado, Minnesota, and Oregon. Additionally, heat stress regulations are being considered in Arizona, New York, Maine, and Maryland. Simultaneously, the movement for a national heat standard has gained momentum. In August 2022, the Natural Resources Defense Council released a report analyzing California employer adherence and the overall effectiveness of the rule, which in turn can inform the development and enforcement of a national regulation. Their key findings:
- Workers in agriculture are affected by heat-related illness and injury more than workers in any other industry. However, heat affects workers across multiple occupations in outdoor settings and indoor environments without adequate cooling, such as construction, outdoor maintenance (e.g., landscaping), indoor maintenance (e.g., pest control), security and parking services, warehouses, and bus and delivery services.
- Many heat penalties imposed on employers by Cal/OSHA stem from complaint-initiated inspections rather than routine inspections.
- Businesses that violate California’s heat illness prevention standard commonly do so more than once.
- Cal/OSHA routinely reduces penalties imposed on employers for violating the heat standard.
- Employers provide inadequate worker training on how to avoid heat-related injuries and illnesses.
- Worker experiences with the California heat standard greatly differ, with vulnerable worker populations such as day laborers and car wash workers bearing the brunt of employer inaction.29
Their key recommendations include:
- Increase funding and recruitment so Cal/OSHA can hire more staff and bilingual inspectors.
- Include more detail in the standard about how employers should provide potentially life-saving elements such as water, rest, shade, and training.
- Better protect workers who report unsafe conditions from retaliation by employers.
- Revise Cal/OSHA’s current citation-reduction policies.30
The report summary concludes, “Overall, the California standard is a good model for OSHA and other states to look to when developing their own heat standard but there is still much room for improvement in how the standard is written and enforced.”
Read the complete report, entitled “Feeling the Heat: How California’s Workplace Heat Standards Can Inform Stronger Protections Nationwide,” at the NRDC website: https://www.nrdc.org/resources/feeling-heat-how-californias-workplace-heat-standards-can-inform-stronger-protections
Resources
- Ventilation as an Essential Control Strategy to Avoid Contagion, by Migrant Clinicians Network with support from National Resource Center for Refugees, Immigrants, and Migrants (NRC-RIM): https://www.migrantclinician.org/resource/ventilation-essential-control-strategy-avoid-contagion.html
- The Western States Pediatric Environmental Health Specialty Unit (PEHSU) has a website with resources for clinicians: https://wspehsu.ucsf.edu
References
Environmental Protection Agency. “How Does Ozone React in the Respiratory Tract?” Health Effects of Ozone in the General Population. Updated 26 August 2022. Accessed 2 March 2023. https://www.epa.gov/ozone-pollution-and-your-patients-health/health-effects-ozone-general-population#respiratory
2 Ibid.
3 California Air Resources Board. Clean-Air Plan for San Joaquin Valley First to Meet All Federal Standards for Fine Particle Pollution. Released 24 January 2019. Accessed 2 March 2023. https://ww2.arb.ca.gov/news/clean-air-plan-san-joaquin-valley-first-meet-all-federal-standards-fine-particle-pollution
4 American Lung Association. Fresno-Madera-Hanford, CA. Accessed 2 March 2023. https://www.lung.org/research/sota/city-rankings/msas/fresno-madera-hanford-ca#pm24
5 Hopper L. USC Children’s Health Study, Now 30 Years Old, Raises Nationwide Awareness of Pollution’s Harms. USCNews. 4 May 2022. https://news.usc.edu/199179/usc-childrens-health-study-now-30-years-old-raises-nationwide-awareness-of-pollutions-harms/
6 Ibid.
7 Yitshak Sade M, Shi L, Colicino E, et al. Long-term air pollution exposure and diabetes risk in American older adults: A national secondary data-based cohort study. Environ Pollut. 2023;320:121056. doi:10.1016/j.envpol.2023.121056
8 Steenhof M, Janssen NA, Strak M, et al. Air pollution exposure affects circulating white blood cell counts in healthy subjects: the role of particle composition, oxidative potential and gaseous pollutants - the RAPTES project. Inhal Toxicol. 2014;26(3):141-165. doi:10.3109/08958378.2013.861884
9 Hew KM, Walker AI, Kohli A, et al. Childhood exposure to ambient polycyclic aromatic hydrocarbons is linked to epigenetic modifications and impaired systemic immunity in T cells. Clin Exp Allergy. 2015;45(1):238-248. doi:10.1111/cea.12377
10 Heft-Neal S, Driscoll A, Yang W, Shaw G, Burke M. Associations between wildfire smoke exposure during pregnancy and risk of preterm birth in California. Environ Res. 2022;203:111872. doi:10.1016/j.envres.2021.111872
11 Reid CE, Brauer M, Johnston FH, Jerrett M, Balmes JR, Elliott CT. Critical Review of Health Impacts of Wildfire Smoke Exposure. Environ Health Perspect. 2016;124(9):1334-1343. doi:10.1289/ehp.1409277
12 Reid CE, Jerrett M, Tager IB, Petersen ML, Mann JK, Balmes JR. Differential respiratory health effects from the 2008 northern California wildfires: A spatiotemporal approach. Environ Res. 2016;150:227-235. doi:10.1016/j.envres.2016.06.012
13 Wettstein ZS, Hoshiko S, Fahimi J, Harrison RJ, Cascio WE, Rappold AG. Cardiovascular and Cerebrovascular Emergency Department Visits Associated With Wildfire Smoke Exposure in California in 2015. J Am Heart Assoc. 2018;7(8):e007492. Published 2018 Apr 11. doi:10.1161/JAHA.117.007492
14 Aguilera R, Corringham T, Gershunov A, Benmarhnia T. Wildfire smoke impacts respiratory health more than fine particles from other sources: observational evidence from Southern California. Nat Commun. 2021;12(1):1493. Published 2021 Mar 5. doi:10.1038/s41467-021-21708-0
15 Neumann JE, Amend M, Anenberg S, et al. Estimating PM2.5-related premature mortality and morbidity associated with future wildfire emissions in the western US. Environ Res Lett. 2021;16(3):10.1088/1748-9326/abe82b. doi:10.1088/1748-9326/abe82b
16 Liu JC, Mickley LJ, Sulprizio MP, et al. Particulate Air Pollution from Wildfires in the Western US under Climate Change. Clim Change. 2016;138(3):655-666. doi:10.1007/s10584-016-1762-6
17 Zhou X, Josey K, Kamareddine L, et al. Excess of COVID-19 cases and deaths due to fine particulate matter exposure during the 2020 wildfires in the United States. Sci Adv. 2021;7(33):eabi8789. Published 2021 Aug 13. doi:10.1126/sciadv.abi8789
18 Garibay C. Valley Towns Are Going to Stay Hotter for Longer. Here’s What That Means for your Health. The Fresno Bee. 26 August 2022. Accessed 2 March 2023. https://www.fresnobee.com/fresnoland/article264860474.html
19 San Joaquin County, CA. The Climate Explorer. Accessed 2 March 2023. https://crt-climate-explorer.nemac.org/climate_graphs/?city=San%2BJoaquin%2BCounty%2C+CA&county=San%2BJoaquin%2BCounty&area-id=06077&fips=06077&zoom=7&lat=37.9175935&lon=-121.1710389&id=days_tmax_gt_100f
20 Fernandez-Bou AS, Ortiz-Partida JP, Pells C, et. Al. Regional Report for the San Joaquin Valley Region on Impacts of Climate Change. California Natural Resources Agency. 2021. Publication number: SUM-CCCA4-2021-003. Accessed 2 March 2023. https://www.energy.ca.gov/sites/default/files/2022-01/CA4_CCA_SJ_Region_Eng_ada.pdf
21 State of California Department of Industrial Relations. Frequently Asked Questions. Piece-Rate Compensation – Labor Code §226.2 (AB 1513). Accessed 2 March 2023. https://www.dir.ca.gov/pieceratebackpayelection/AB_1513_FAQs.htm
22 Mix J, Elon L, Vi Thien Mac V, et al. Hydration Status, Kidney Function, and Kidney Injury in Florida Agricultural Workers. J Occup Environ Med. 2018;60(5):e253-e260. doi:10.1097/JOM.0000000000001261
23 Seda CH. Masks for Fires: Kathryn Conlon, PhD, MPH Analyses new California Emergency Wildfire Smoke Regulation For Outdoor Workers. Clinician to Clinician: Migrant Clinicians Network Blog. 25 September 2019. Accessed 2 March 2023. https://www.migrantclinician.org/blog/2019/sep/masks-fires-kathryn-conlon-phd-mph-analyses-new-california-emergency-wildfire-smoke
24 Rosa MJ, Just AC, Kloog I, et al. Prenatal particulate matter exposure and wheeze in Mexican children: Effect modification by prenatal psychosocial stress. Ann Allergy Asthma Immunol. 2017;119(3):232-237.e1. doi:10.1016/j.anai.2017.06.016
25 Wright RJ. Advancing Exposomic Research in Prenatal Respiratory Disease Programming. Immunol Allergy Clin North Am. 2023;43(1):43-52. doi:10.1016/j.iac.2022.07.008
26 Pagán-Santana M, Liebman AK, Seda CH. Deepening the Divide: Health Inequities and Climate Change among Farmworkers. J Agromedicine. 2023;28(1):57-60. doi:10.1080/1059924X.2022.2148034
27 Ventilation as an Essential Control Strategy to Avoid Contagion. Migrant Clinicians Network. Accessed 2 March 2023. https://www.migrantclinician.org/resource/ventilation-essential-control-strategy-avoid-contagion.html
28 Benisek A. What Is a Corsi-Rosenthal Box? WebMD. 29 January 2023. Accessed 2 March 2023. https://www.webmd.com/allergies/corsi-rosenthal-box
30 Adewumi-Gunn T, Constible J. Feeling the Heat: How California’s Workplace Heat Standards Can Inform Stronger Protections Nationwide. Natural Resources Defense Council. 14 September 2022. Accessed 2 March 2023. https://www.nrdc.org/resources/feeling-heat-how-californias-workplace-heat-standards-can-inform-stronger-protections
29 Ibid.