Community Health Workers (CHWs) are critical clinical care team members who act as a link and liaison between a health center or other site of health care provision, and communities with shared backgrounds who are served by that health center. Also called promotoras or promotores de salud, health promoters, or outreach educators, CHWs can translate clinical information, like preventative care, into appropriate non-technical messages tailored for the community.
Community health workers are community leaders and change agents who create a link between the community and the health center. Health center staff can more easily learn of values and practices related to health, changes in the demographics, needs, or perspectives of the community when they have a CHW on the ground. This trusted link between the health center and the community can prove vital during emergencies or other periods of uncertainty when trust can increase the likelihood of the effective distribution of information and resources.
However, unlike other members of the care team, CHWs do not have a nationally standardized education or training, which complicates efforts to assess their overall impact. This lack of standardization hinders concrete analysis, as individual studies on CHWs are not comparable, given that each study may feature CHWs with different educational backgrounds.1 Additionally, each health center integrates CHWs in different ways into their clinical care team; health sites with excellent integration, education, and support of CHWs likely experience higher rates of desired outcomes.2 Despite these inconsistencies, many studies on CHW utilization point to improved health behaviors, better health outcomes, and reduced costs, indicating that despite the various CHW models in place, CHWs consistently positively impact their communities. Given that they often support migratory and seasonal agricultural workers (MSAWs) and their families, CHW integration is highly recommended.
ECHO as a Model Project ECHO is a learning framework developed by the University of New Mexico that has been used around the world to support training in health care. Project ECHO, stands for “Extension for Community Healthcare Outcomes,” augments typical virtual learning by giving health care providers direct access to subject matter experts, with a focus on brief lectures, case-based learning, and sharing of promising practices. “Even with the best technology, webinars don’t always provide close connection. It’s the connection, the learning from each other, that is the core of ECHO and MCN’s approach to communities of learning,” explained Alma Galván, MHC, Director of Community Training and Engagement for MCN. See how other organizations are using the ECHO model.
To support the integration of CHWs and ensure high-quality in-depth education specifically designed for CHWs, Migrant Clinicians Network (MCN) offers year-round educational opportunities and support via virtual communities of learning available in Spanish and English. Many CHWs working in Spanish-speaking communities are first-language Spanish speakers themselves. Most struggle to find training and education tailored to their educational needs and preferences, and the health needs and language preferences of their communities. Further complicating their education, many – particularly those serving MSAWs – live in highly rural areas with few options for connection and mentoring. MCN’s small-group learning sessions, including our popular six-week Diabetes ECHO series, give CHWs the information, resources, examples, networking or network connections, and tools in their preferred language. (See sidebar on ECHO as a model.) During these communities of learning, CHWs benefit from connection with other CHWs and promising practice sharing, access to experts in their fields, and materials in various literacy levels. Materials and training in their language remove the need for translation and reduce the possibility of miscommunication or misunderstandings on core health concepts. Additionally, MCN augments the ECHO model to include participatory evaluation, regularly adjusting the trainings in response to the expressed needs of the cohort. As a result of this broad support, CHWs in MCN communities of learning show a significant self-reported increase in understanding of key areas around diabetes management, control, treatment, and prevention for communities like Spanish-speaking MSAWs. The 2024 cohort of the MCN Diabetes ECHO is an example of effective CHW education and training.
In 2024, MCN provided the six-session Diabetes ECHO series for the seventh consecutive year. The series topics included: diabetes type 2 general information, nutrition and diabetes, mental health and diabetes, treatments and medications for diabetes, and community involvement and education. From over 100 applicants, 31 individuals were accepted and 26 comprised the final group. About 78% of participants indicated that Spanish was their first language. Educational attainment and age were extremely diverse. Most had been in their current position for between one and five years. Participants were from across the United States, from Washington State to Florida. Several joined from Puerto Rico.
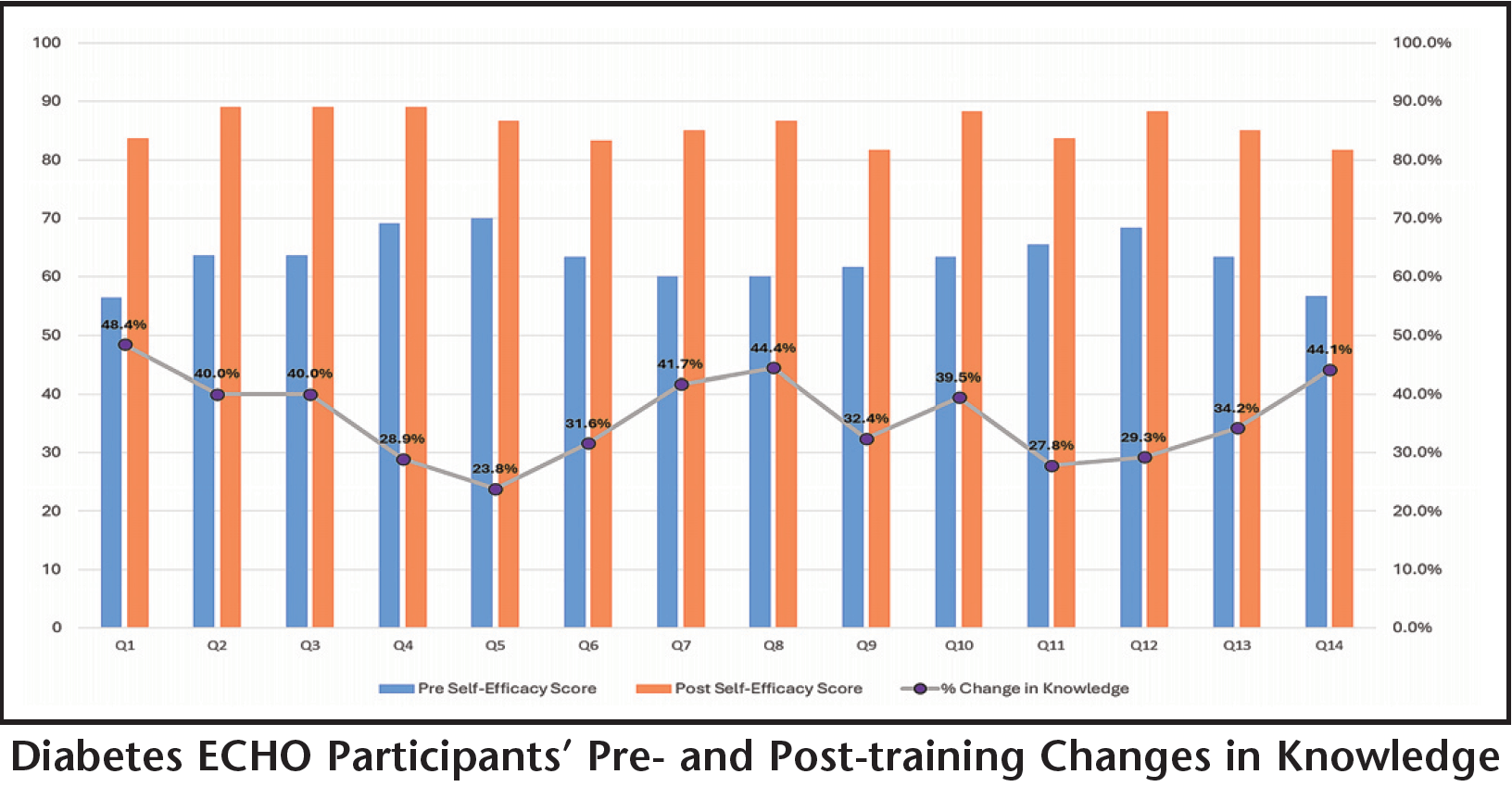
To gauge the effectiveness of the trainings, MCN asked participants to submit a pre- and post-training self-efficacy questionnaire. The questions revolved around the gain of knowledge, confidence, or ability for a variety of practices that are conducive to successful diabetes self-management. Participants were given access to the online questionnaire upon the conclusion of the six-part series. They were asked to think retrospectively about their abilities, knowledge, or skills, both prior to participating in the series and after they had participated in the series.
Diabetes Among MSAWs In 2023, the American Diabetes Association surveyed 16,913 MSAWs. Age-adjusted self-reported diabetes prevalence was at 10.8% among MSAWs with stable households and even higher, at 13.51%, among MSAWs who move to follow harvests. Importantly, the study noted that MSAWs who move for the harvest and did not recently access health care “had 83% lower odds of reporting known diabetes.” As the diabetes diagnosis was self-reported rather than clinically validated, this result suggests that many mobile workers with poor health care access are unaware they have diabetes, the authors concluded. The authors of the survey also noted that newly arrived MSAWs who are foreign-born may be healthier than those who have lived full-time in the US for longer periods of time, and that farm work may select for fitter individuals given the “grueling manual labor” – both factors may possibly contribute to a lower true diabetes prevalence. Without a clinical screening to measure blood sugars in participants, the true burden of diabetes among workers remains unclear.
Citation: Olson RM, Nolan CP, Limaye N, Osei M, Palazuelos D. National Prevalence of Diabetes and Barriers to Care Among U.S. Farmworkers and Association With Migrant Worker Status. Diabetes Care. 2023;46(12):2188-2192. doi:10.2337/dc23-0960
Scoring for each question was based on a 1 to 5 Likert scale. Questions assessed the CHW participants’ knowledge on explaining to patients how behaviors or habits can cause diabetes, ability to help patients establish an exercise routine, analyze with patients the benefits of a healthy diet and give appropriate advice, recognize acute complications of diabetes, and more.
Increases in knowledge were indicated by participants across all 14 questions. Highest rates of change were seen in ability to obtain the general medical history of patients (48% increase), with a total of six questions out of 14 showing an increase in knowledge of at least 40%. The overall reported increase in knowledge was 36.2%.
Every year, MCN receives hundreds more applicants for our Diabetes ECHO series than can be accommodated in the small 30-person community of learning. In response to the ongoing need, MCN has developed an alternative diabetes ECHO community of learning, in a shorter format, and open to more individuals.
“Our clinical network of support staff, including CHWs/promotores de salud, are often hard pressed to find education around type 2 diabetes in Spanish that addresses the specific needs of their patient population, i.e. Spanish-speaking workers and/or MSAWs who may move from location to location for purposes of work,” said Martha Alvarado, Manager of Online Education for MCN.
Based on the popularity of our Diabetes ECHO series, and the expressed need of our constituents, MCN has developed a shorter four-session series on Type 2 diabetes that will address the most popular diabetes self-management topics, including nutrition and mental health.
Learn more about the series and register on MCN’s website: https://www.migrantclinician.org/webinars/upcoming
Citations
1 Pinto D, Carroll-Scott A, Christmas T, Heidig M, Turchi R. Community health workers: improving population health through integration into healthcare systems. Curr Opin Pediatr. 2020;32(5):674-682. doi:10.1097/MOP.0000000000000940
2 McCarville E, Martin MA, Pratap P, Pinsker E, Seweryn SM, Peters KE. Understanding critical factors associated with integration of community health workers into health and hospital systems. J Interprof Care. 2024;38(3):507-516. doi:10.1080/13561820.2023.2183183