Migrant Clinicians Network Announces New Co-Chief Medical Officer, Laszlo Madaras, MD, MPH
By Claire Hutkins Seda, Writer, Migrant Clinicians Network, Managing Editor, Streamline
This year, Migrant Clinicians Network welcomed a new Co-Chief Medical Officer, Laszlo Madaras, MD, MPH, who has joined longtime CMO Ed Zuroweste, MD in the many efforts that MCN spearheads to advance health justice for the mobile poor. Dr. Madaras comes to MCN with decades of experience in health justice, international medicine, and mobile health, and has swiftly become an integral part of MCN’s hardworking staff.
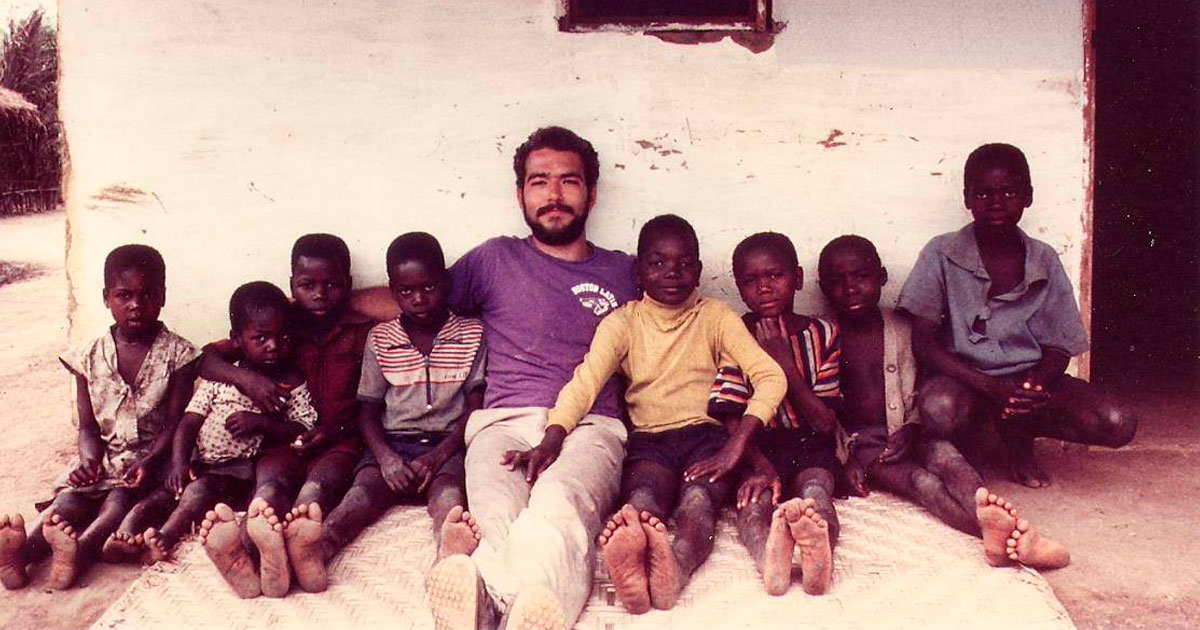
Dr. Madaras started on the track to a medical research career during his undergraduate years at Dartmouth, where he researched muscular dystrophy at the Boston Biomedical Research Institute. Luckily for his many future patients, Dr. Madaras discovered a preference for people over test tubes. A turning point came after college, when he joined the Peace Corps, which brought him to the Democratic Republic of Congo (then known as Zaire). Honing his French and picking up Swahili and Kikongo, Dr. Madaras worked on a tilapia fish farming project. He also encountered international doctors for the first time, which fueled a goal to work on the frontlines as a primary care provider serving underserved patients.
When he returned, he took a job at the Environmental Protection Agency while prepping for medical school. At the EPA, he learned the ins and outs of environmental policy, in particular working on removing carbon tetrachloride from food additives and grains. When he made his way to Tufts Medical School, he was 28. He pursued a combined MD/MPH four-year degree. “I pretty much went in with the goal of doing primary care — and I never turned back,” he noted.
During his final year of residency, he was contacted by an international aid group, American Refugee Committee, asking if he would join them to work in Rwanda. It was 1994, and the country was deep in the aftermath of a horrendous genocide. “Since I’d been a Peace Corps volunteer, I knew the language, I knew the geography of the area, and I could drive a Land Rover, they said I could come for just three months,” instead of the more typical six-month deployment.
He arrived in a refugee camp of 170,000 refugees. He was one of the youngest doctors there; his mentors were international disaster veterans, previously working in the war fields of Cambodia and Vietnam. He worked six to 12 hours a day, triaging people to the correct spot, with separate tents for cholera, malaria, dysentery, meningitis, and more.
The heaviness of war was hard for Dr. Madaras as a young doctor. “On one of my first days, we had about 500 deaths in 24 hours. The old veterans said it was a good day,” he said. Deaths were declining as more time passed; when he left three months later, less than a hundred people were dying each day. “People were very generous, very kind during my time there in the Peace Corps. It was very hard to see this switch where people could be so incredibly cruel to each other. I had such good memories in the Peace Corps just ten years before! I saw the best and the worst of Africa in the same region, within ten years.”
As for many who return from such harrowing experiences, it was challenging for Dr. Madaras to fold back into his final year of residency. His first rotation upon return was in dermatology. “The derm patients’ concerns were real, although some were ‘just cosmetic,’ but it was very different than dealing with machete lacerations,” Dr. Madaras said. “I tried to recognize that, as a family doctor, I also need to know about skin ailments. But it was kind of a shock to go from one extreme to the other.”
Upon graduation, he was accepted into the National Health Service Corps loan repayment program, a popular program offered by the Health Resources and Services Administration (HRSA) that places clinicians in underserved areas in exchange for loan repayments, thereby reducing a new clinician’s debt while gaining much-needed primary care services in underserved areas like in Federally Qualified Health Centers around the country.
“I had to serve in a physician-shortage area — and that’s when I met Dr. Ed Zuroweste,” Dr. Madaras recalled. After a summer in the Dominican Republic on a vaccination program, Dr. Madaras could add Spanish to his list of languages in which he could communicate with patients. That brought his spoken languages up to seven, as he also had Hungarian and German under his belt.
“Seven languages is a huge plus for a health center — and he used all those languages at our health center. He worked with our mobile population from day one,” Dr. Zuroweste recalled. He jumped at the chance of having Dr. Madaras at Keystone Health Center in Pennsylvania, which Dr. Madaras joined in 1996. The two physicians, with similar interests in medicine, hit it off. Dr. Zuroweste was impressed by the international experience he brought at such an early stage in his career. “I once saw him at a street fair where five patients came up to him separately, all speaking different languages. I saw people watch him do that and think, ‘What the heck is going on?’”
Over the years, Dr. Madaras and Dr. Zuroweste continued to cross paths, even after Dr. Madaras left Keystone family medicine to become a hospitalist and in-patient doctor. When volunteering with the local state department of health clinic, Dr. Madaras would work with mobile agricultural workers, referring those who needed case management to Dr. Zuroweste for what became Health Network, and giving him an early peek into MCN’s work.
Starting in 2002, Dr. Madaras began joining Dr. Zuroweste for some of his trips to the rural mountains of Honduras with fourth-year medical students from Johns Hopkins and elsewhere. The trips serve to give future doctors a low-tech highly needed international medicine experience. Dr. Madaras even brought his children, “for helping in the work and for them to see how much of the world really lives. It’s important to have compassion and understanding for how people live in the world,” he noted.
As he grew more involved in work with mobile populations, he was invited to present for the World Conference of Family Doctors where he talked about mobile populations and control of infectious diseases like tuberculosis and HIV. While he continued to enjoy the diversity of work as a community health doctor — “I was delivering babies! In a small town, I got to do everything under the umbrella of family medicine,” he said — his work with the mobile poor in his community continued. For the last eight years, Dr. Madaras cut back to strictly inpatient hospitalist, for better work-life balance. But in 2012, Dr. Madaras added outpatient medicine back to his schedule, as a TB physician with the Pennsylvania State Health Department, another place where he joined Dr. Zuroweste in work for the underserved. Last year, Dr. Zuroweste approached Dr. Madaras to see if he’d want to work with MCN as Dr. Zuroweste eases into retirement. “He’s the perfect fit for MCN,” Dr. Zuroweste admits, who is thrilled that Dr. Madaras has joined on and has begun a long transition during which both doctors share the role of Chief Medical Officer. Dr. Madaras currently works about 10 days a month at the hospital, another day with the TB clinics, and spends the rest of the time in a number of pursuits, including ramping up his work for MCN.
Dr. Madaras is very positive about the longer transition. “I’ve had enough experience with leadership change in institutions to know that everything slows down if the new guy has to figure everything out without overlap. But MCN needs to keep moving forward. Ed is still here with the guiding hand and I’m absorbing the way things work,” he said.
“It’s an ideal way to transition with a less-than-ideal outside environment in health care. We will continue to be challenged in the coming years, and I’m hoping to help move MCN forward as we figure out which way we need to go.”
Read this article in the Fall 2017 issue of Streamline here!
Sign up for our eNewsletter to receive bimonthly news from MCN, including announcements of the next Streamline.